What is Eosinophilic Esophagitis?
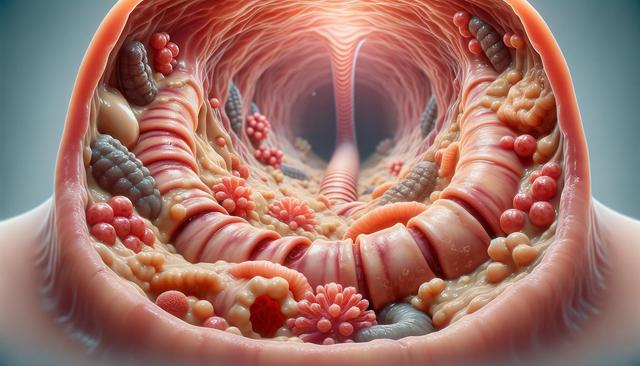
Eosinophilic Esophagitis, often abbreviated as EoE, is a chronic inflammatory disease of the esophagus. It is characterized by an elevated number of eosinophils, a type of white blood cell, in the esophageal tissue. These cells are not typically found in the esophagus, and their presence is usually a response to allergens or acid reflux. Over time, this inflammation can lead to narrowing of the esophagus, difficulty swallowing, and food getting stuck, particularly in children and young adults. Although the exact cause is not yet fully understood, EoE is believed to be triggered by allergic reactions to certain foods or environmental allergens.
Individuals with EoE may experience a range of symptoms, which can vary in severity and frequency. Common symptoms include:
- Difficulty swallowing (dysphagia)
- Chest pain that is not related to heartburn
- Food impaction (food getting stuck in the esophagus)
- Persistent heartburn or acid reflux that does not improve with medication
- Feeding difficulties and failure to thrive in children
These symptoms often lead to misdiagnosis, as they resemble those of other gastrointestinal conditions such as GERD (gastroesophageal reflux disease). Therefore, accurate diagnosis through endoscopy and biopsy is essential.
Causes and Risk Factors
The exact cause of Eosinophilic Esophagitis is still being studied, but it is widely considered to be an immune-mediated disease. Research suggests that EoE is often linked to food and environmental allergens. When the body’s immune system reacts to these allergens, it mistakenly sends eosinophils to the esophagus, leading to inflammation and tissue damage. Several risk factors have been associated with the development of EoE:
- Family history of allergic diseases
- Personal history of asthma, eczema, or allergic rhinitis
- Male gender (EoE is more common in males than females)
- Being diagnosed at a young age (commonly during childhood or early adulthood)
Because of these associations, EoE is often considered part of a group of allergic disorders. Understanding these risk factors can help in identifying at-risk individuals and implementing early intervention strategies.
Diagnosis and Testing
Diagnosing Eosinophilic Esophagitis typically requires a combination of clinical evaluation, endoscopic examination, and histological analysis. Since EoE symptoms can mimic other gastrointestinal conditions, a thorough diagnostic process is essential. The key steps in diagnosing EoE include:
- Upper endoscopy: A thin, flexible tube with a camera is used to examine the esophagus.
- Biopsy: Small tissue samples are taken from the esophagus and examined under a microscope for the presence of eosinophils.
- Allergy testing: Skin prick tests or blood tests may be conducted to identify possible food or environmental allergens that may be triggering the condition.
In some cases, patients may be asked to follow an elimination diet where suspected foods are removed, then gradually reintroduced to identify triggers. It is important that patients work closely with a gastroenterologist and an allergist to ensure an accurate diagnosis and appropriate management plan.
Treatment and Management
There is currently no cure for Eosinophilic Esophagitis, but several treatment approaches can help manage symptoms and reduce inflammation. Treatment typically involves a combination of dietary modifications, medications, and in some cases, endoscopic procedures. The most common strategies include:
- Dietary therapy: Removal of specific food allergens from the diet. The most common allergens include dairy, wheat, eggs, soy, nuts, and seafood.
- Proton pump inhibitors (PPIs): These medications reduce acid production in the stomach and may decrease eosinophil levels in some patients.
- Topical corticosteroids: Swallowed steroids, such as fluticasone or budesonide, can reduce inflammation in the esophagus without the systemic effects of oral steroids.
- Dilation: In cases where the esophagus has become significantly narrowed, endoscopic dilation may be used to stretch and widen the esophagus to relieve symptoms.
Management of EoE often requires long-term monitoring and adjustment of therapy. Regular follow-ups with a healthcare provider are important to assess treatment effectiveness and modify strategies as needed.
Living with Eosinophilic Esophagitis
Living with EoE can present challenges, especially when it comes to dietary restrictions and ongoing symptom management. However, with proper care and support, individuals with EoE can lead full and active lives. It’s essential for patients and caregivers to stay informed and engaged in the management process. Some helpful practices include:
- Working with a registered dietitian to ensure nutritional needs are met despite food restrictions
- Maintaining a symptom diary to track potential triggers and treatment responses
- Staying updated on new research and treatment options through reputable sources
- Joining support groups or connecting with others who have EoE for shared experiences and advice
Adapting to life with EoE may require changes in eating habits and lifestyle, but many people find relief and improved quality of life with the right combination of treatments. Awareness and education are key to effectively managing this condition.



Leave a Reply