Understanding Kidney Disease: An Overview
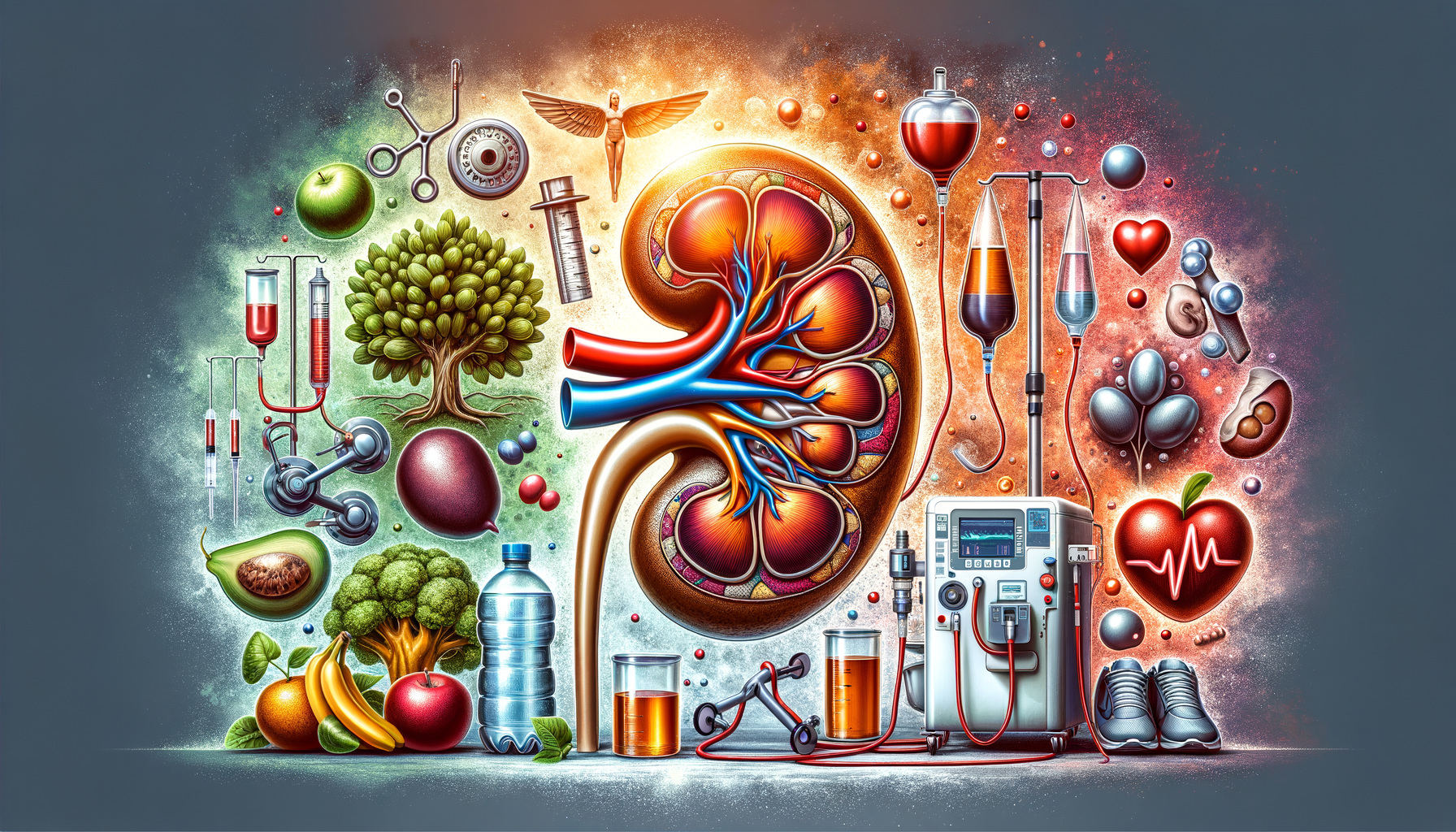
Kidney disease, often referred to as renal disease, involves the gradual loss of kidney function over time. The kidneys are vital organs responsible for filtering waste products and excess fluids from the blood, which are then excreted in urine. When the kidneys are damaged, waste products and fluids can build up in the body, leading to various health issues.
There are several types of kidney disease, with chronic kidney disease (CKD) being the most common. CKD is typically caused by conditions like diabetes and high blood pressure, which gradually impair kidney function. Acute kidney injury, on the other hand, occurs suddenly and is often reversible with prompt treatment.
It’s essential to understand the risk factors associated with kidney disease to take preventative measures. These include:
- Diabetes
- High blood pressure
- Heart disease
- Smoking
- Obesity
- Family history of kidney disease
Early detection and management are crucial in slowing the progression of kidney disease and maintaining a healthy lifestyle.
Conservative Management: Lifestyle and Medication
For those diagnosed with early stages of kidney disease, conservative management can be an effective approach. This method focuses on lifestyle modifications and medication to manage symptoms and slow disease progression.
Dietary changes are a cornerstone of conservative management. Patients are often advised to reduce salt intake, limit protein consumption, and maintain a balanced diet rich in fruits and vegetables. Staying hydrated is also essential, but fluid intake may need to be monitored based on individual health conditions.
Medications play a crucial role in managing underlying conditions that contribute to kidney disease. For instance:
- Blood pressure medications, such as ACE inhibitors, help control hypertension.
- Diabetes medications manage blood glucose levels.
- Cholesterol-lowering drugs reduce cardiovascular risk.
Regular monitoring of kidney function through blood and urine tests is vital to assess the effectiveness of conservative management and make necessary adjustments to the treatment plan.
Dialysis: A Lifesaving Procedure
As kidney disease progresses to advanced stages, dialysis may become necessary. Dialysis is a medical procedure that performs the function of the kidneys by removing waste products and excess fluids from the blood when the kidneys are no longer able to do so efficiently.
There are two main types of dialysis: hemodialysis and peritoneal dialysis. Hemodialysis involves using a machine to filter the blood, typically done at a dialysis center several times a week. Peritoneal dialysis, on the other hand, uses the lining of the abdomen to filter blood and can often be done at home.
Choosing between these options depends on various factors, including the patient’s lifestyle, medical condition, and personal preference. Both methods aim to improve quality of life and extend survival, but they require strict adherence to treatment schedules and dietary restrictions.
While dialysis is a critical treatment for advanced kidney disease, it is not a cure. Patients on dialysis must continue to work closely with their healthcare team to manage their condition and explore other potential treatment options.
Kidney Transplantation: A New Lease on Life
For many patients with end-stage kidney disease, a kidney transplant offers a chance for a longer, healthier life. A kidney transplant involves surgically placing a healthy kidney from a donor into the patient’s body, where it can take over the functions of the failed kidneys.
Transplants can come from living donors, often relatives or friends, or deceased donors. While living donor transplants generally have better outcomes, both options are viable and can significantly improve the recipient’s quality of life.
After a successful transplant, patients typically experience improved energy levels, fewer dietary restrictions, and a reduced need for dialysis. However, they must take immunosuppressive medications for life to prevent the body from rejecting the new kidney.
While a kidney transplant is a major surgical procedure with potential risks, it remains a highly effective treatment for suitable candidates. The decision to pursue transplantation should involve thorough discussions with healthcare providers to understand the benefits and challenges.
Complementary Therapies: Supporting Conventional Treatment
In addition to standard medical treatments, some patients explore complementary therapies to support their kidney health. These therapies do not replace conventional treatment but can enhance overall well-being and help manage symptoms.
Common complementary therapies include:
- Acupuncture, which may help alleviate pain and improve energy levels.
- Herbal supplements, though it’s crucial to consult with healthcare providers to avoid interactions with prescribed medications.
- Mind-body practices, such as yoga and meditation, which can reduce stress and improve mental health.
While these therapies can offer additional support, it’s essential for patients to discuss any complementary approaches with their healthcare team to ensure they are safe and appropriate for their specific condition.
Ultimately, managing kidney disease requires a comprehensive approach that combines medical treatment, lifestyle changes, and, when appropriate, complementary therapies to achieve the best possible health outcomes.



Leave a Reply