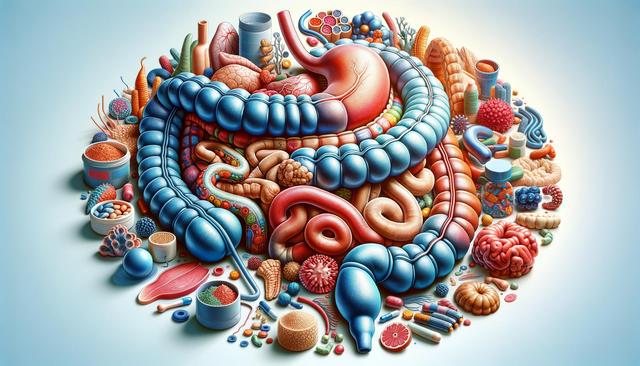
What Is Crohn’s Disease?
Crohn’s disease is a type of inflammatory bowel disease (IBD) that causes inflammation in the digestive tract, most commonly affecting the end of the small intestine and the beginning of the colon. However, it can impact any part of the gastrointestinal tract, from the mouth to the anus. The condition is chronic, meaning it persists over a long period and often requires ongoing management. Though its exact cause is unknown, researchers believe it involves a combination of genetic predisposition, immune system dysfunction, and environmental factors. Unlike some other digestive disorders, Crohn’s disease can lead to deep ulcerations and even thickening of the intestinal wall.
Common symptoms include:
- Persistent diarrhea
- Abdominal pain and cramping
- Unintended weight loss
- Fatigue
- Fever
Because symptoms vary widely in severity and location, Crohn’s is sometimes difficult to diagnose. It can also mimic other conditions, such as irritable bowel syndrome (IBS) or ulcerative colitis, requiring thorough evaluation by a healthcare provider.
Causes and Risk Factors
While the root cause of Crohn’s disease remains unclear, several contributing factors have been identified. Genetics play a significant role, as individuals with a family history of Crohn’s are more likely to develop the disease themselves. The immune system also contributes by mistakenly attacking healthy gut bacteria, triggering inflammation. Additionally, environmental factors, such as diet, smoking, and stress, may exacerbate symptoms or trigger flare-ups.
Major risk factors include:
- Age: Most people are diagnosed before age 30
- Family history: Having a close relative with the disease increases risk
- Smoking: Tobacco use is linked to more severe symptoms and complications
- Geographic location: Higher incidence in urban and northern climates
Understanding these risk factors can help individuals and healthcare providers take preventative measures or monitor for early signs of the disease.
Diagnosis and Testing
Diagnosing Crohn’s disease typically involves a combination of medical history, physical examinations, and various diagnostic tests. Because no single test can definitively diagnose the condition, a step-by-step approach is often used. Blood tests may reveal signs of inflammation or anemia, while stool tests can exclude infections and detect blood or inflammation markers.
Common diagnostic procedures include:
- Colonoscopy: Allows direct visualization of the colon and terminal ileum with tissue biopsies
- Endoscopy: Used to examine the upper gastrointestinal tract
- Imaging studies: CT scans and MRIs help detect inflammation and complications like fistulas or abscesses
- Capsule endoscopy: A small camera swallowed by the patient provides images of the small intestine
Early and accurate diagnosis is vital for initiating treatment and preventing complications such as intestinal strictures or malnutrition.
Treatment Options
There is no cure for Crohn’s disease, but various treatments can help manage symptoms and maintain remission. The choice of treatment depends on the severity, location of the disease, and individual response to therapies. Medications are often the first line of defense and are aimed at reducing inflammation, suppressing the immune response, and alleviating symptoms.
Common treatment approaches include:
- Anti-inflammatory drugs: Such as aminosalicylates and corticosteroids
- Immune system suppressors: Including biologics and immunomodulators
- Antibiotics: To treat secondary infections or complications
- Dietary changes: Tailored nutrition plans can help reduce flare-ups and ensure nutrient intake
In some cases, surgery may be necessary to remove damaged portions of the gastrointestinal tract or to address complications. While surgery doesn’t cure the disease, it can greatly improve quality of life when other treatments are ineffective.
Living With Crohn’s Disease
Managing Crohn’s disease involves more than just medical treatment; it requires a comprehensive lifestyle approach. Patients often benefit from working with a multidisciplinary team that includes gastroenterologists, dietitians, and mental health professionals. Understanding personal triggers—such as specific foods or stress—is key to minimizing flare-ups and maintaining remission.
Helpful strategies for daily management include:
- Maintaining a food journal to identify triggers
- Eating smaller, more frequent meals
- Staying hydrated
- Engaging in stress-reducing activities like yoga or meditation
- Joining support groups for emotional and social encouragement
With proper management, many individuals with Crohn’s disease are able to lead fulfilling and active lives. Staying informed and maintaining open communication with healthcare providers can make a significant difference in long-term outcomes.



Leave a Reply